A new hope/dream for women with advanced maternal age who postponed mothering a child due to marriage or career plans: Pre-implantation genetic screening/testing (PGS/PGT);
Why does the chance of getting pregnant decrease as the age of women increase and the risk of having an unhealthy baby increase?
Nowadays, IVF technology is improving very fast. Such improvement, especially in the era of genetics, permits us to assess the viability of the embryo in the most objective way. Such assessment obviously lets us to choose the most viable single embryo for transfer.
The contemporary goal of IVF is take-home, healthy, singleton baby. In order to achieve this goal, it is mandatory to have the most reliable, robust, objective tool to select the best embryo. Currently, PGS/PGT fulfills this goal to a great extent.
With female ageing, time-to-spontaneous pregnancy is prolonged with increased risk of spontaneous miscarriage. Normally, women produce new eggs only in utero and no new egg production in ovaries occurs following birth. During the reproductive life span, an egg undergoes 2 maturation divisions to be mature and ready to be fertilized. However, those eggs that are used in later reproductive life span (greater than 36-yr old) are more prone to develop errors either during the first and/or second maturation division. With such errors, the eggs will be endorsed with abnormal number of chromosomes (e.g. 22, 24, 25), rather than the correct number of 23. The odds of error at female age 36-38 is around 50-55%; these figures are 60-65%, 75% and 100% at female ages of 40, 42-43 and 46, respectively. Obviously, fertilization of such abnormal oocytes will result in abnormal embryos failing to implant, miscarry or gestations with abnormal number of chromosomes, such as Down syndrome (mongolism, trisomy 21). It is of interest that such abnormal oocytes/embryos cannot be discernible from normal, healthy ones based on their morphologic appearance. Hence, PGS/PGT permits us to select the most viable embryo with correct number of chromosomes without relying on morphology, which might be misleading.
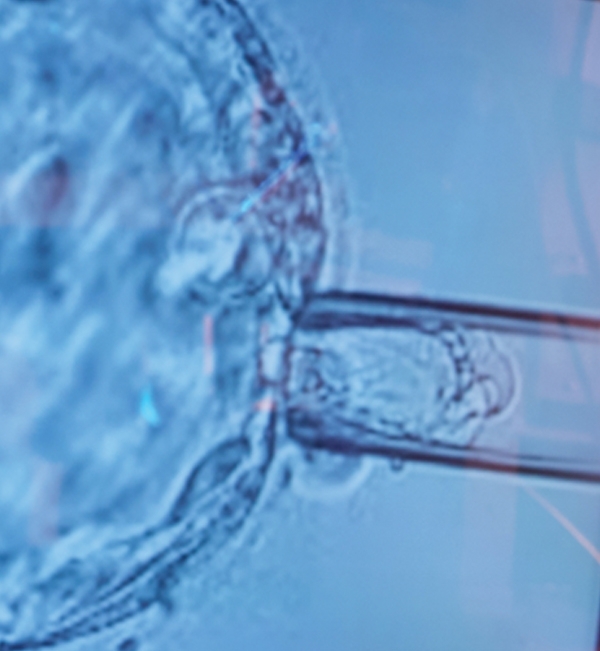
Thanks to the method of PGS/PGT, embryos are frozen after biopsied from the part, which will form the placenta called trophectoderm, and cell samples are sent to the genetic lab and the screen is provided for all of the chromosomes including 22 pairs somatic and 2 sex chromosomes.
For genetic analysis, we collaborate with igenomix, a worldwide known respectful genetic laboratory with good reputation. Igenomix uses the most valid genetic platform, called the next generation sequencing platform with high resolution (NGS-hr).
Once a normal/healthy embryo is reported by the genetic testing, embryo transfer is planned.
With PGS/PGT, the female age and the number of previous failed cycles lose their importance. Therefore, with the availability of such filtrated embryos, we only transfer one embryo, regardless of female age and number of previous failed cycles. The reason for that is the pregnancy rates with PGS/PGT with single embryo transfer in this difficult patient population is around 70%! Obviously, PGS/PGT would not correct an abnormal embryo, but rather permits us to select the most viable embryo that would maximize her chance of live birth. The other 2 advantages of PGS/PGT are significantly decreased risk of miscarriage (8-9%) and nearly elimination of twins. When one considers the very high risk of miscarriage in standard IVF (12% at 36-38; 20-25% at 40; 45-50% at 42-43-yr old), such significant reduction of miscarriage in all female age groups is striking! Finally, avoiding multiple pregnancies is another advantage of PGS/PGT.
Consequently, the live birth rate rates around 55% are achieved in women 42-45-yr old.
It is of critical importance that the embryo biopsy is done at the blastocyst stage (day 5 or 6; very rarely Day 7). Day 3 biopsy (3 days after oocyte retrieval), should not be performed.
The main reason for performing PGS/PGT at our Center is advanced maternal age (greater than 38-yr old). PGS/PGT may also be performed to select the best embryo in patients with recurrent implantation failure or recurrent miscarriage, although firm scientific evidence is lacking for these 2 conditions.
We have a successful PGS/PGT program since March 2015, having performed more than 500 cycles. The live birth rate per single embryo transfer with PGS/PGT, at our Center, in such difficult patients is around 55%.