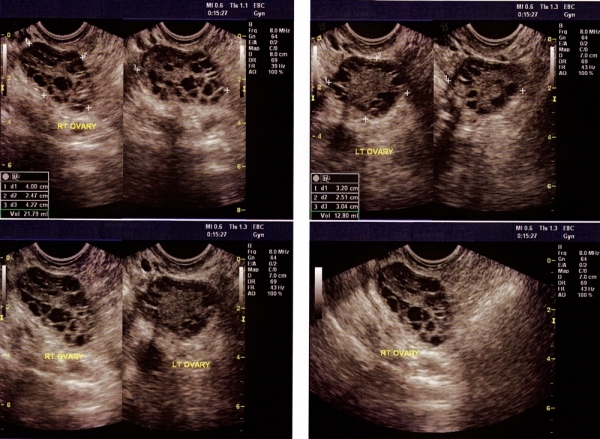
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder in reproductive age period. The frequency of PCOS is around 15-17%. PCOS is characterized by menstrual irregularity characterized by i) less than 9 menses per year, ii) androgen excess-either increased serum androgen (male hormone) levels or skin findings of increased androgen levels characterized by hirsutism (increased hair growth), oily skin, acne and hair loss and iii) polycystic ovarian appearance at ultrasonography (more than 12 antral follicles of 2-9 mm in each ovary).
The frequency of being overweight and obesity is increased in women suffering from PCOS. Furthermore, excess fat is deposited on the low abdominal region (male-type obesity) in such cases.
Insulin resistance is characteristic in patients affected by PCOS. Therefore, impaired glucose tolerance as well as type-2 diabetes are increased in women with PCOS. Most probably, the risk of hypertension and coronary heart disease may also be increased in such women. Therefore, one should keep in mind that PCOS is a metabolic disorder, associated with long-term risk factors including type-2 diabetes, hypertension and coronary heart disease.
Since the majority of these patients do not ovulate on themselves, there is no progesterone (ovulation hormone) production. Since progesterone opposes estrogen action on the inner lining of uterus and with the lack of progesterone in PCOS patients with long-lasting ignored cases, the thickness of the inner lining might be increased. In such cases, even the risk of cancer of the inner lining might be increased. Therefore, it is essential that these patients should have medications to have regular cycles.
PCOS is the most common reason for infertility due to the absence of ovulation. When fertility is desired in such women, medications are used to induce ovulation. Treatment options in patients having difficulty in getting pregnant are;
- The first-line treatment is an oral drug, named letrozole. It is an oral medication, easy to use and cheap. There is no need for follow-up with ultrasonography during this treatment. This drug is started as 2.5 mg (1 tablet) per day; based on the ovarian response the dose might be increased, if necessary. With this treatment in 6 months, 80% of the patients ovulate and 40% conceive.
- The second-line treatment is low-dose daily injection therapy. In order to stimulate ovulation, by using daily rather small doses of gonadotrophins (Gonal-F, Puregon, Menogon, Menopur, Fostimon or Merional), 1 or 2 follicles are aimed to be grown. Final shut injection is performed when the size of follicle(s) reaches 17-18 mm. With this approach, ovulation is induced in 95% of the patients. The pregnancy rate per treatment cycle is around 20-23%. Although not mandatory, we also perform intrauterine insemination (IUI-putting the washed sperm into the uterus 40 hours after the final shot by a catheter under ultrasonographic guidance). Following 3-4 cycles of such treatment, if the patient fails to conceive, IVF treatment is recommended.
- The third-line treatment is IVF. Pregnancy rates achieved with IVF in such patients are very reassuring at least as good as compared to those patients not suffering PCOS. A freeze-all approach is usually undertaken in patients with PCOS undergoing IVF; for this approach fresh embryo transfer is not performed and all the eligible blastocysts are frozen on Day 5/6. Such an approach has 2 advantages: 1) with frozen replacement transfer, the live birth rate per transfer is enhanced compared to fresh transfer; 2) the risk of ovarian hyperstimulation syndrome (OHSS) is nearly eliminated. Since, in usual cases, good number of blastocysts are frozen, “one and done” is achieved, in other terms many couples can complete their family (2-3 children) with only one ovarian stimulation/egg retrieval.